newsletters
Nursing shortages and vacancies have always been an issue in healthcare operations, but every year it is becoming more concerning, and even crippling, in hospitals across the country.
Unfortunately, there is no one-size-fits-all solution when it comes to staffing shortages. However, there are proven best practices that can make a difference!
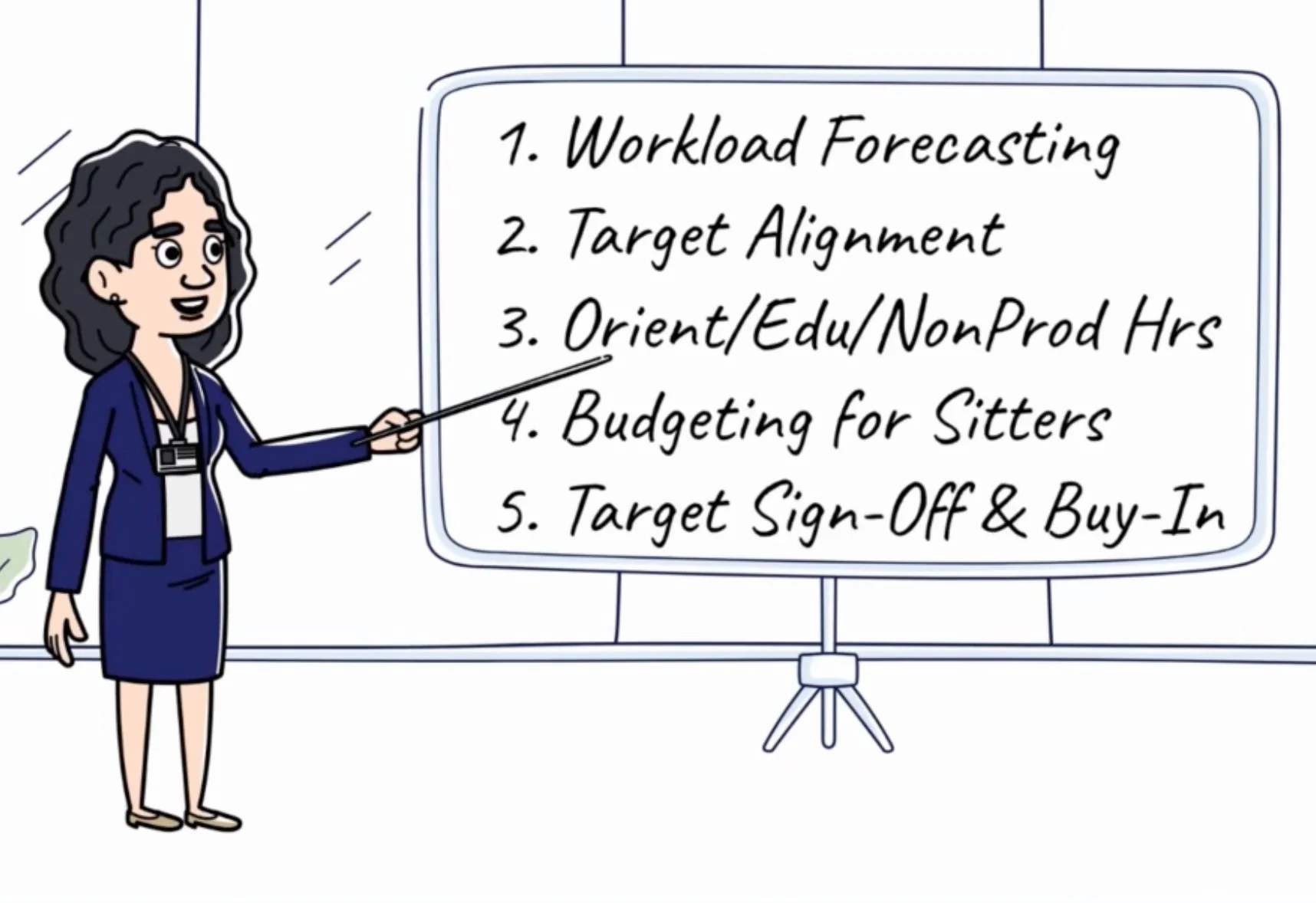
Uninformed labor cost projections can make or break your budget, but it can be tough to know where to start - which is why we've prioritized 5 key areas of focus for you! If you're looking for a hospital FTE budget study guide, keeping reading!
Have you ever wondered how finance sets a department's budget each year? While most explanations we've heard sound quite complex, the truth is quite simple.
There are only 3 ways to set a productivity target: Run Rate, Benchmark, and Zero-Base
Leaders struggling with their target often ask this question and most are unable to get a straight answer - perhaps because the person they are asking isn't sure. This common complaint inspired us to share this newsletter and we hope it helps!
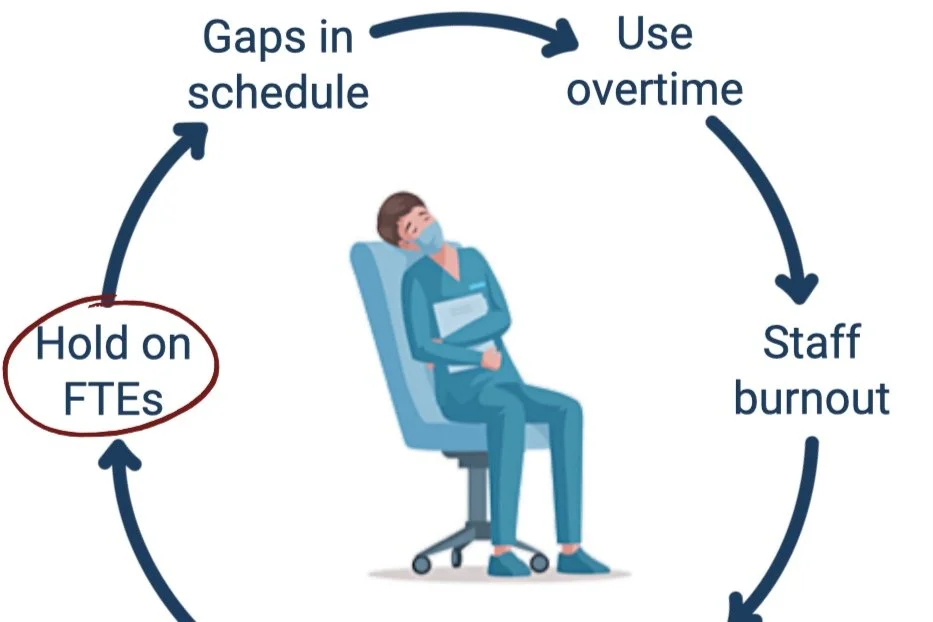
How do organizations accurately determine the number of Full-Time Equivalents (FTEs) needed to fill staff schedules without requiring overtime?
If you’ve ever worked on this problem, you know that hiring 30 FTEs does NOT imply 30 FTEs will be worked. This means FTE totals taken from the HRIS system are unreliable (no, we aren’t referencing nonproductive time, although it also must be considered when calculating productive availability)!
To truly understand staffing commitment, we must review historically worked hours for each team member. A team member’s commitment is defined as the weekly hours they have agreed to work. As an example, 0.9 FTE RNs are hired to work 36 hours per week (typically in a 3x12 shift format).
Analyzing FTE availability begins with comparing this agreed-upon FTE commitment with actual worked hours.
How confident are you that your managers and directors are prepared to lead their teams?
Are you sure they have the tools they need to do a great job?
If so, you’re ahead of most. In healthcare we have SO many opportunities to improve, but we commonly trip over the finish line when it comes to execution. When it comes to change management, accountability is key, but support is often overlooked.
We observe poor leadership preparedness all the time – seeing it everywhere from academic medical centers to community hospitals – so we designed a solution– or at least part of one. Whether it is information about industry best practices or simply supporting sustainable growth through 1:1 coaching a resource to support improvement for new and tenured leaders should be available to them.
Both support and accountability are required to drive results, so understanding your role in this respect is critically important.
Support includes activities like education, 1:1 time, tools, communication, setting expectations, and other activities that help individuals achieve their goals. Accountability, on the other hand, facilitates individual responsibility including leveraging reports to ask tough questions, ensuring deadlines are met and that rules are enforced.
In the education field, our job is almost 100% support. What about yours?
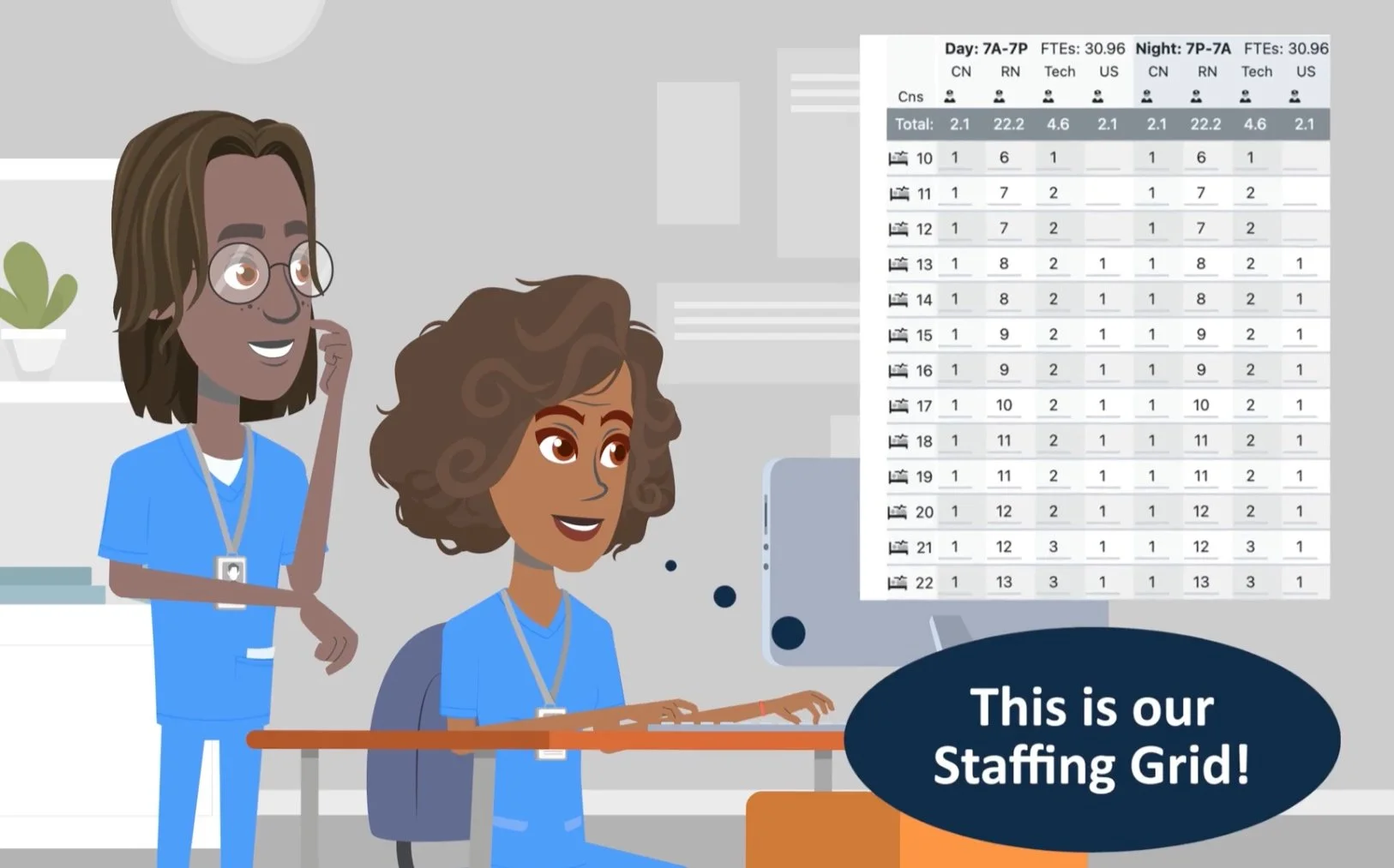
Staffing grids connect clinical and financial guidelines in a way that effectively supports sustainable operations.
We aren't sure how long they've been around, but we would assume that the first staffing grid is older than anyone reading this, given how beautifully simple and impactful these little pieces of paper can be.
Does your nursing unit's staffing grid align with the budget financially? Are your nursing units staffing in alignment with their grids? How do you know? How do you ensure consistent nursing ratios between units? Across multiple hospitals in a health system?
Is the ER solely responsible for boarders at your hospital? If so, #youredoingitwrong!
While patients with admission orders waiting to go upstairs are physically in the ER, the drivers of their delay has very little to do with the ER itself. The truth about boarders is that they are primarily driven by inefficient processes on the inpatient side, while the ER pays the price.
According to the CDC, more than 1.5 million would-be ER patients leave without being seen each year in the US. Exacerbated by the pandemic, the Left Without Being Seen (LWBS) rate has skyrocketed, leading to significant lost revenue for hospitals who desperately need it to support staffing levels. Ensuring patients receive care when they need it is a critical part of supporting the communities we serve. Design a plan to keep both patients and finances healthy with proven ER best practices.
Many organizations implement float pools to help cover unexpected gaps in schedules, but without a thoughtful approach and proper planning, they routinely fail – sometimes costing their organizations millions per month in avoidable spend with no end in sight.
Departments request float pool resources for all open shifts, regardless of the reason. However, successful labor leaders understand that each type of resource demand - due to vacancy, maternity leave, seasonal peak volumes, etc - requires a specific support strategy.
How does your hospital manage position approvals? We've observed 3 methods: Hiring to budgeted FTEs, approvals based on productivity performance, or customized department FTE hire targets based on total annual projected labor spend. Hire targets provide a specific FTE value for departments to maintain by considering volume-driven monthly FTE needs and total annual labor cost. For best results, start with the most cost effective option and make adjustments from there by carefully considering the operational feasibility of flexing up. Remember: the best way to address chronic vacancies is to hire ahead of turnover!
Hospitals define premium pay as any rate of pay above the base employed rate. Premium pay can include shift bonuses, weekend differentials, overtime, contract labor, and more.
Premium pay is of vital importance when staffing 24/7 patient care operations. By design, it acts as a financial incentive where needed to support balanced shifts and ensures we have the right staff, in the right place, at the right time, to provide optimal patient care.
Nurse vacancies and contract labor rates have soared in the post-pandemic environment. As a result, many hospitals are currently evaluating alternative care delivery models to support the staffing ratios needed to provide quality patient care and retain staff. This newsletter reviews four alternative care delivery model options, ideas to attract applicants, and considerations for successfully implementing a change to your current care delivery model.
While monthly performance tracking to budgeted goals is critical to the success of any business, hospitals tend to have more complex drivers of budget variance than other industries. Because workforce constitutes 50-60% of hospital spend and is widely considered the most controllable expense, labor is often the focus of budget variance conversations.
Department productivity drives hospital FTE performance to budget. High performing organizations proactively and thoughtfully cascade realistic FTE budgets to department productivity goals. After working with many hospitals and health systems over the years, our team has identified the top 5 labor budgeting practices that drive favorable FTE performance. These tactics significantly minimize budget risk by ensuring all risks can be mitigated through department action plans.
Labor benchmarks are commonly used in healthcare to inform leaders about opportunities to gain efficiencies. However, we often see leaders incorrectly use benchmark as a management tool. When this happens, we miss the opportunity to dig deeper to understand the opportunity and create a plan to improve. This can leave department leaders exasperated with chasing quarterly moving targets, but worse still, this approach can invite short sighted decisions that ultimately pose risks to patient care.
If you’ve worked in healthcare operations leadership for more than 18 months, you have likely heard the term “Benchmark.” If you’ve led a department for more than 5 years, you’ve likely been on the wrong side of a benchmark comparison (or know a poor soul who has). This newsletter explores the data review required to ensure accurate submissions, ultimately supporting useful performance comparisons for all participants.
Traditional on-call programs impact department culture and finances. Call-back premium pay rates increase department labor expenses, and the demands of the call schedule can contribute to poor staff satisfaction, high turnover, and difficulty recruiting. In many cases, alternative solutions are more advantageous than the traditional on-call model.
Contract labor resources are a true asset to healthcare organizations when utilized appropriately and managed well. However, many organizations find it challenging to align contract labor to their staffing needs while controlling overall labor expenses.
High performing organizations quantify anticipated needs for vacancies, leave of absence support, and seasonal workload volume fluctuations while ensuring contract labor is never used inappropriately through attentive management.
Across the country, hospitals have been forced to close their doors due to revenue headwinds and increasing costs due to the COVID 19 pandemic. All are working to closely manage costs to keep their doors open for the communities they serve.
Perhaps the most approachable and impactful strategy to reduce cost while improving care is demand matching – the process of reviewing staff schedules and patient workload volumes to align staff with volume by hour of day. Even if you’ve done this in the past, it’s important to reevaluate as patient volume patterns have shifted in hospitals across the country.
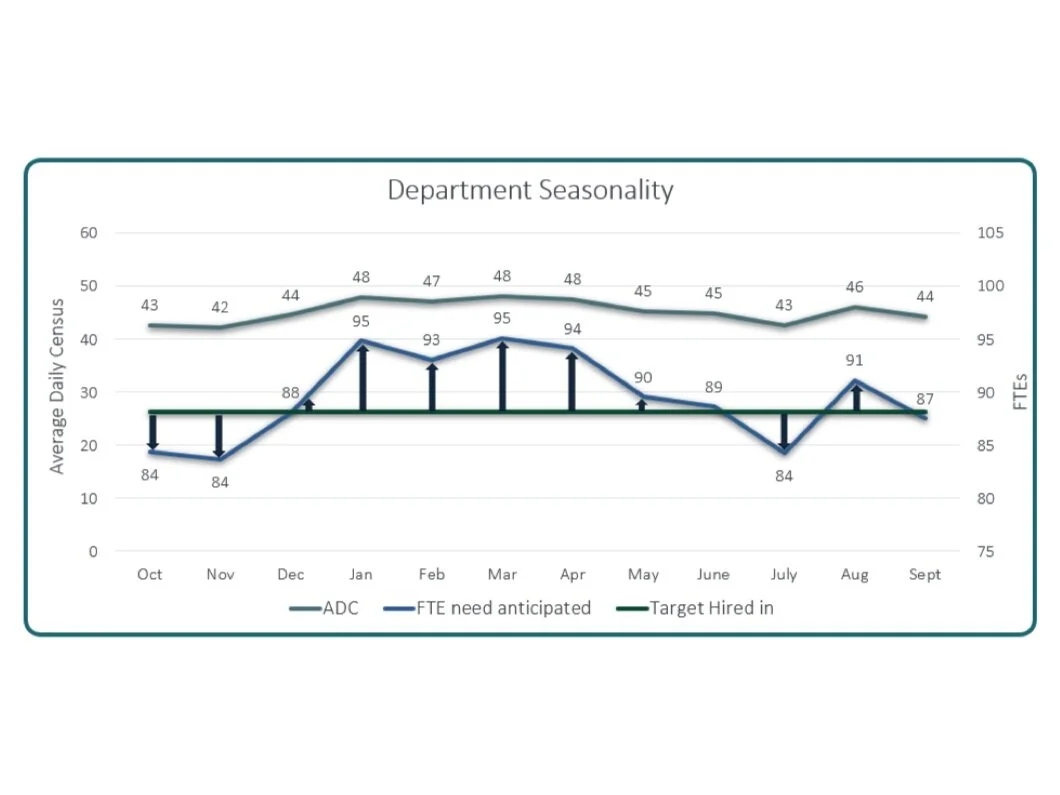
Experienced leaders know the turnaround time for hiring and orienting staff creates a greater vacancy burden than is typically seen on paper. When staff are unavailable to work, we rely on premium labor such as overtime or travelers to care for our patients, which can adversely impact our culture, outcomes, and hospital finances.
Hiring ahead is a strategy that allows us to quantify the true vacancy burden and hire the perfect number of FTEs and reduce avoidable premium pay.
Productivity targets help hospitals balance resource requirements with financial goals by budgeting specific hours for the workload in each department. The process of setting productivity targets can present a challenge to both nursing and finance leaders as they work together to identify the ideal goal. By using zero based staffing models, industry leaders ensure that the right staff are in the right place at the right time.
Top performing hospital leaders are always searching for innovative ways to reduce the cost of healthcare without adversely impacting care and services provided. Labor spend constitutes over half of total hospital expenses and is widely considered the most controllable expense. Daily productivity management can help hospitals reduce expenses without having to furlough or lay off staff members. A successful strategy includes two primary components: increased performance visibility through daily reporting and managing improvement through department action plans to remedy missed targets.
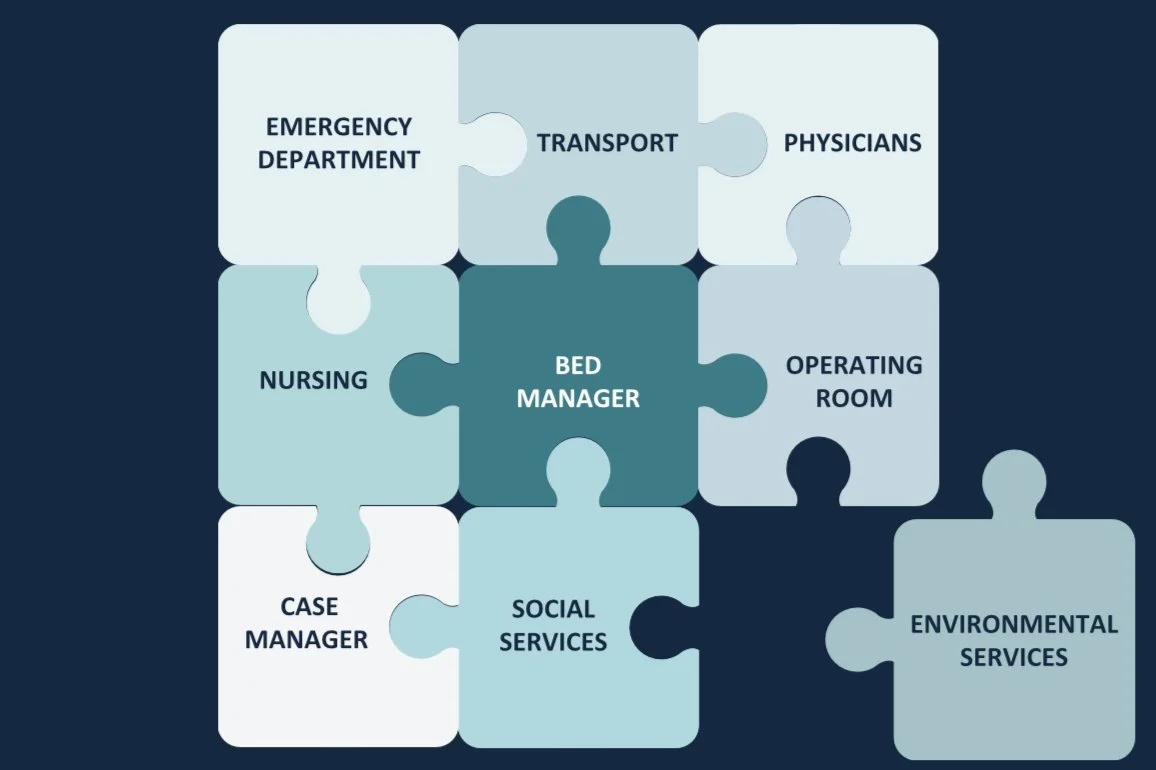
Hospitals across the country are faced with daily bed management challenges. With ED admissions typically peaking between 3:00pm to 7:00pm, PACU admissions between 12:00pm to 4:00pm, and inpatient discharges between 6:00pm to 8:00pm, it is easy to see why capacity challenges exist. Now, more than ever, capacity management requires thoughtful consideration to maximize appropriate utilization of beds, staff, and services. CCC team member, Susie Law shares key tactics for maximizing hospital capacity in this article.
Revenue degradation experienced due to the COVID-19 pandemic is impacting hospital finances across the country. Suspension of elective surgeries and procedures threatens the viability of many healthcare organizations. After decades of experience in the for-profit sector, our team has summarized some of the top impact expense management strategies. Continue reading for a high level view and check out our article for more details.
Extended wait times, driven by throughput challenges, cause patients to leave the Emergency Room without being seen. Efficiency requires coordination among many departments and team members. Each department plays a vital role in ER throughput, contributing to patient experience. From lab and imaging results, to patient registration, to EVS room turnaround time, there are many components which impact department efficiency. Routine reviews of department metrics are necessary to identify throughput pain points that impact both patient and staff satisfaction.
Staffing grids are planning tools that assign the appropriate amount of staff to care for the number of patients on the unit. Effective staffing grids support care guidelines and productivity by integrating with budget, hiring plans, and scheduling systems. Annual approval by the CFO and CNO is important, as the types of patients cared for on the unit can vary over time.
Across the country, Emergency Departments are actively working to manage both revenue and cost by reducing patients who leave without being seen, managing labor spend, and improving core measure performance. Aligning staff with volume by hour of day is challenging, but necessary to address these critical issues.
Many organizations struggle to staff to monthly workload fluctuations. Flexing up and down is hard work, but proven strategies exist to proactively plan for changing workload to optimize labor spend. In Healthcare Business Today, Cara discusses high level strategies for seasonal staffing.